Get Quick Relief Now: 3 Way – Effective Treatment Options for Plantar Fasciitis at HirePhysio.com
Plantar fasciitis and other foot problems can be a source of significant discomfort and pain. These conditions can interfere with daily activities and negatively impact quality of life. Fortunately, with the help of a qualified physiotherapist, many of these conditions can be treated effectively. At HirePhysio.com, we provide a convenient platform to help you find and hire the best physiotherapist near you. Our network of experienced and licensed physiotherapists specialize in treating a wide range of foot problems, including plantar fasciitis, Achilles tendinitis, bunions, and more. With HirePhysio.com, you can find the right physiotherapist near you, to help alleviate your foot pain and improve your overall mobility and wellness.
PLANTAR FASCIITIS AND OTHER FOOT PROBLEMS
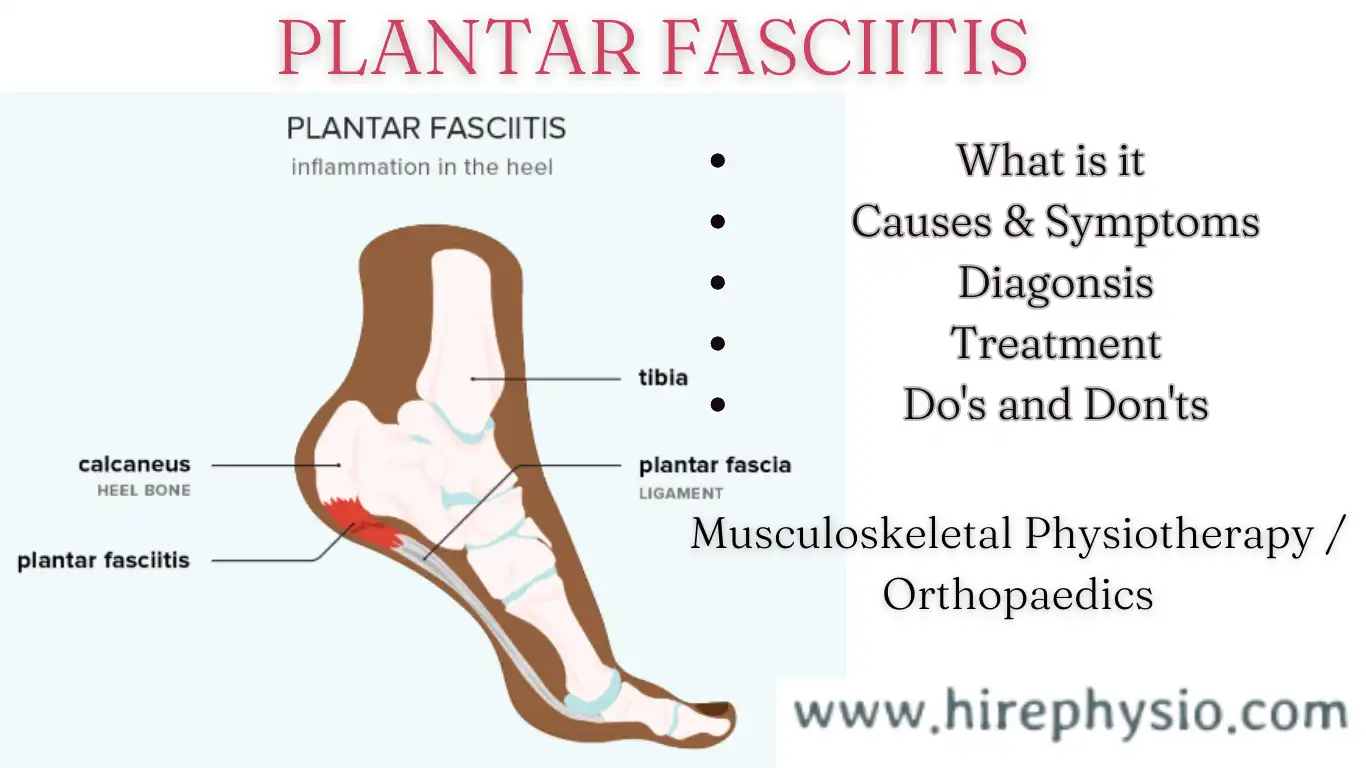
Plantar fasciitis is a common foot problem that is caused by inflammation of the plantar fascia, a thick band of tissue that runs along the bottom of the foot. It is often characterized by heel pain, especially in the morning when first getting out of bed or after sitting for a long time.
There are several other foot problems that can cause pain and discomfort, including:
- Achilles tendinitis – Inflammation of the Achilles tendon that connects the heel to the calf muscle.
- Bunions – A bony bump that forms at the base of the big toe, causing it to point inward and the joint to stick out.
- Morton’s neuroma – A thickening of the tissue around the nerve that runs between the third and fourth toes, causing pain and numbness.
- Plantar warts – Small, painful growths on the sole of the foot caused by a virus.
- Hammer toes – A condition where the toes bend downward at the middle joint, causing pain and discomfort.
Treatment for these foot problems may vary, but generally includes rest, ice, stretching, physical therapy, and the use of supportive footwear. In more severe cases, medication or surgery may be necessary.
WHO GETS PLANTAR FASCIITIS ?
Plantar fasciitis can affect anyone, but it is most commonly seen in middle-aged people, particularly those who are on their feet for extended periods of time, such as athletes, soldiers, and people who work in jobs that require standing for long periods. Some other factors includes:
- Age: Plantar fasciitis can affect anyone, but it is more commonly seen in middle-aged people.
- Occupations: Individuals who are on their feet for extended periods of time, such as athletes, soldiers, and people who work in jobs that require standing for long periods, are at a higher risk of developing plantar fasciitis.
- Obesity: Being overweight or obese can increase the risk of developing plantar fasciitis.
- Foot structure: People with flat feet or high arches are more likely to develop plantar fasciitis.
- Tight muscles: Tight calf muscles can put extra strain on the plantar fascia, leading to plantar fasciitis.
- Footwear: Wearing shoes with poor arch support or that do not fit properly can contribute to the development of plantar fasciitis.
- Gender: Plantar fasciitis is more common in women than men.
WHAT ARE THE CAUSES OF PLANTAR FASCIITIS
The exact cause of plantar fasciitis is not fully understood, but there are several factors that can contribute to its development. Here are some of the common causes of plantar fasciitis:
- Overuse: Repetitive activities that put stress on the plantar fascia, such as running or jumping, can cause micro-tears in the tissue, leading to inflammation and pain.
- Tight muscles: Tight calf muscles can put extra strain on the plantar fascia, increasing the risk of developing plantar fasciitis.
- Foot structure: People with flat feet or high arches are more likely to develop plantar fasciitis because these foot structures can cause an uneven distribution of weight on the feet, leading to excessive stress on the plantar fascia.
- Obesity: Being overweight or obese can increase the stress on the plantar fascia, leading to inflammation and pain.
- Footwear: Wearing shoes with poor arch support or that do not fit properly can contribute to the development of plantar fasciitis.
- Age: Plantar fasciitis is more common in middle-aged people because the plantar fascia becomes less flexible and more prone to injury as we age.
It’s important to note that plantar fasciitis is often caused by a combination of these factors, rather than just one singular cause.
WHAT ARE THE SYMPTOMS OF PLANTAR FASCIITIS
The most common symptom of plantar fasciitis is pain on the bottom of the heel, which can be sharp or dull. The pain is typically worse in the morning when taking the first few steps out of bed or after prolonged periods of sitting or standing. Other symptoms of plantar fasciitis may include:
- Pain that worsens with activity, especially activities that involve running or jumping.
- Tenderness or stiffness in the arch of the foot.
- Swelling in the bottom of the foot.
- Pain that improves with rest.
- Pain that is more severe after exercise rather than during it.
It’s important to note that not all heel pain is caused by plantar fasciitis, and a healthcare professional should be consulted for a proper diagnosis and treatment plan.
DIFFERENT WAYS TO DIAGNOSIS PLANTAR FASCIITIS
There are several ways that plantar fasciitis can be diagnosed. Here are some of the most common methods:
- Physical examination: A healthcare professional will examine the foot, looking for signs of tenderness, redness, or swelling in the heel area. They will also check for limited range of motion in the ankle and foot.
- Imaging tests: X-rays or other imaging tests, such as an MRI, may be ordered to rule out other causes of heel pain, such as a stress fracture or nerve entrapment.
- Ultrasound: An ultrasound may be used to examine the plantar fascia and determine if it is thickened or inflamed.
- Diagnostic injections: In some cases, a diagnostic injection of local anesthesia or corticosteroids may be used to confirm the diagnosis of plantar fasciitis and provide temporary pain relief.
- Foot pressure analysis: A foot pressure analysis may be used to assess the distribution of pressure on the feet while standing or walking, which can help identify any issues with foot structure or gait that may contribute to plantar fasciitis.
WHAT ARE THE TREATMENT FOR PLANTAR FASCIITIS
Treatment for plantar fasciitis typically involves a combination of self-care measures and medical interventions. Here are some common treatments:
- Rest and activity modification: Resting the affected foot and avoiding activities that exacerbate pain is a critical part of treatment. Low-impact activities such as swimming or cycling may be recommended as an alternative.
- Ice therapy: Applying ice to the affected area can help reduce pain and inflammation.
- Stretching and strengthening exercises: Exercises that stretch and strengthen the plantar fascia and surrounding muscles can help alleviate pain and prevent recurrence.
- Footwear modifications: Wearing shoes with good arch support and cushioning can help reduce stress on the plantar fascia.
- Orthotics: Custom-made shoe inserts can help correct any underlying foot abnormalities and improve foot function.
- Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) may be recommended to reduce pain and inflammation.
- Night splints: Wearing a splint that keeps the foot in a flexed position while sleeping can help stretch the plantar fascia and reduce morning pain.
- Physical therapy: Working with a physical therapist can help develop an individualized treatment plan and provide guidance on exercises and self-care measures.
In more severe cases, medical interventions such as corticosteroid injections or shock wave therapy may be recommended. Surgery is rarely necessary but may be considered in cases that do not respond to other treatments.
HOW MUCH TIME IT TAKES TO TREAT PLANTAR FASCIITIS BY PHYSICAL THERAPY
The length of time it takes to treat plantar fasciitis with physical therapy can vary depending on several factors, such as the severity of the condition and how well the patient responds to treatment. In general, physical therapy for plantar fasciitis involves a combination of stretching, strengthening, and other exercises to help alleviate pain and promote healing.
Treatment typically lasts several weeks to a few months, with regular appointments scheduled every week or two. However, some patients may require more or less treatment depending on their individual needs. It’s important to follow the treatment plan prescribed by your physical therapist and to continue practicing the exercises and self-care measures recommended even after symptoms improve to prevent recurrence.
HOW TO MAKE PLANTAR FASCIITIS HEAL FASTER OR RECOVER FASTER
While the recovery time for plantar fasciitis can vary depending on the severity of the condition and other factors, there are several things you can do to help speed up the healing process:
- Rest the affected foot: Rest is essential for allowing the plantar fascia to heal properly. Avoid activities that exacerbate pain and consider low-impact exercises such as swimming or cycling as an alternative.
- Apply ice: Applying ice to the affected area can help reduce pain and inflammation. Use an ice pack for 15 to 20 minutes at a time, several times a day.
- Stretch and strengthen exercises: Regularly performing exercises that stretch and strengthen the plantar fascia and surrounding muscles can help alleviate pain and promote healing.
- Wear proper footwear: Wearing shoes with good arch support and cushioning can help reduce stress on the plantar fascia and promote healing.
- Use orthotics: Custom-made shoe inserts can help correct any underlying foot abnormalities and improve foot function, which can help promote healing.
- Get physical therapy: Working with a physical therapist can help develop an individualized treatment plan and provide guidance on exercises and self-care measures that can help promote healing.
- Consider medical interventions: In more severe cases, medical interventions such as corticosteroid injections or shock wave therapy may be recommended.
It’s important to consult with a healthcare professional for a proper diagnosis and treatment plan. Following their recommendations and committing to self-care measures can help promote faster recovery from plantar fasciitis.
WHAT ARE THE PHYSIOTHERAPY TREATMENT FOR PLANTAR FASCIITIS
Some physiotherapy treatments for plantar fasciitis are as follows:
Initial Assessment:
The first step in physiotherapy treatment for plantar fasciitis is an initial assessment. The physiotherapist will take a detailed history of your symptoms and perform a physical examination to determine the cause and extent of your condition. They may also use diagnostic imaging such as ultrasound to confirm the diagnosis.
Education and Advice:
The physiotherapist will provide education and advice on how to manage your symptoms, including the importance of rest, ice therapy, and wearing proper footwear. They will also advise you on activities to avoid that may aggravate your symptoms.
Manual Therapy:
Manual therapy techniques such as massage, soft tissue mobilization, and joint mobilization may be used to help alleviate pain, improve flexibility, and promote healing.
Stretching Exercises:
Stretching exercises can help alleviate pain and improve flexibility in the plantar fascia and surrounding muscles. Your physiotherapist will provide guidance on how to perform these exercises safely and effectively.
Strengthening Exercises:
Strengthening exercises can help improve foot function and prevent recurrence of plantar fasciitis. Your physiotherapist will prescribe exercises specific to your individual needs and level of function.
Gait Analysis:
Gait analysis involves analyzing the way you walk and identifying any abnormalities that may contribute to your condition. Your physiotherapist may use video analysis or other methods to assess your gait and provide recommendations for corrective exercises or modifications to your footwear.
Orthotics:
Custom-made orthotics can help correct any underlying foot abnormalities and improve foot function, which can help promote healing. Your physiotherapist may recommend orthotics as part of your treatment plan.
Electrotherapy:
Electrotherapy techniques such as ultrasound, electrical stimulation, and laser therapy may be used to help reduce pain and inflammation and promote healing.
Home Exercise Program:
Your physiotherapist will provide you with a home exercise program to continue your rehabilitation outside of your therapy sessions. Following your home exercise program can help promote faster recovery and prevent recurrence of plantar fasciitis.
Overall, physiotherapy treatment for plantar fasciitis is typically individualized based on the patient’s specific needs and goals. By working with a physiotherapist and following a comprehensive treatment plan, patients can improve their symptoms and return to their regular activities.
WHAT ARE THE CHIROPRACTOR TREATMENT FOR PLANTAR FASCIITIS
Chiropractors can provide several treatment options for plantar fasciitis. Here are some common chiropractic treatments for plantar fasciitis:
Spinal and Extremity Adjustments:
Chiropractors use manual adjustments to correct misalignments in the spine and extremities. These adjustments can help improve foot and ankle function and alleviate pain associated with plantar fasciitis.
Soft Tissue Therapy:
Chiropractors may use soft tissue techniques such as massage, myofascial release, and trigger point therapy to help alleviate pain and promote healing in the plantar fascia and surrounding muscles.
Stretching and Strengthening Exercises:
Chiropractors may prescribe stretching and strengthening exercises to improve foot and ankle function and prevent recurrence of plantar fasciitis. These exercises can help stretch the plantar fascia and strengthen the muscles that support the foot and ankle.
Kinesiology Tape:
Kinesiology tape is a flexible tape that can be applied to the skin to provide support and reduce pain. Chiropractors may use kinesiology tape to support the plantar fascia and alleviate symptoms.
- Foot Orthotics:
Chiropractors may prescribe custom-made foot orthotics to help correct any underlying foot abnormalities and improve foot function, which can help alleviate pain and promote healing.
Lifestyle and Nutritional Advice:
Chiropractors may also provide lifestyle and nutritional advice to help improve overall health and reduce inflammation, which can contribute to plantar fasciitis. They may recommend changes to your diet, exercise routine, and sleep habits to promote healing.
WHAT ARE THE ACCUPRESSURE OR ACCUPUNTURIST TREATMENT FOR PLANTAR FASCIITIS
Acupressure and acupuncture are both holistic therapies that involve the application of pressure or needles to specific points on the body to help alleviate pain and promote healing. Here are some common acupressure and acupuncture treatments for plantar fasciitis:
Acupressure Massage:
Acupressure massage involves applying pressure to specific points on the feet, ankles, and legs to help alleviate pain and promote healing in the plantar fascia and surrounding muscles. This type of massage can also help improve circulation and reduce inflammation.
Acupuncture:
Acupuncture involves the insertion of thin needles into specific points on the body to help stimulate the body’s natural healing processes. In the case of plantar fasciitis, acupuncture may be used to promote circulation, reduce inflammation, and alleviate pain.
Herbal Medicine:
Acupuncturists may also recommend the use of herbal medicine to help alleviate pain and promote healing. Herbs such as turmeric, ginger, and boswellia may be recommended for their anti-inflammatory and pain-relieving properties.
Lifestyle Advice:
Acupressure and acupuncture practitioners may also provide lifestyle advice to help improve overall health and reduce inflammation, which can contribute to plantar fasciitis. They may recommend changes to your diet, exercise routine, and sleep habits to promote healing.
WHAT ARE YOGA TREATMENT FOR PLANTAR FASCIITIS
Yoga is a holistic practice that can help improve flexibility, strength, and balance in the body. It can also be a helpful complementary therapy for plantar fasciitis. Here are some common yoga treatments for plantar fasciitis:
Stretching:
Yoga poses such as Downward-Facing Dog, Standing Forward Bend, and Crescent Lunge can help stretch the plantar fascia and alleviate pain. These poses can also help stretch the calves, hamstrings, and hips, which can contribute to plantar fasciitis.
Strengthening Exercises:
Yoga poses such as Tree Pose, Warrior II, and Chair Pose can help strengthen the muscles that support the feet and ankles. These poses can also help improve balance and stability in the lower body.
Relaxation Techniques:
Yoga also incorporates relaxation techniques such as deep breathing and meditation, which can help reduce stress and promote healing. Reducing stress can be particularly helpful for those with plantar fasciitis, as stress can contribute to inflammation and pain.
Mindful Movement:
Yoga emphasizes mindful movement and paying attention to the body’s sensations. By practicing yoga mindfully, individuals with plantar fasciitis can learn to move in a way that is gentle and supportive of their feet and ankles.
WHAT DO’S AND DON’TS ADVICE IS GIVEN TO PATIENTS HAVING PLANTAR FASCIITIS
Here are some general do’s and don’ts advice given to patients having plantar fasciitis:
Do’s:
- Do stretch your feet and calves regularly to help prevent tightness and strain on the plantar fascia.
- Do wear supportive shoes with good arch support and cushioning to help alleviate pressure on the plantar fascia.
- Do rest your feet and avoid high-impact activities that can aggravate the condition.
- Do seek treatment from a qualified healthcare professional such as a physical therapist, chiropractor, or acupuncturist to help alleviate symptoms and promote healing.
- Do maintain a healthy weight to reduce stress on the plantar fascia.
Don’ts:
- Don’t ignore the pain, as this can lead to further damage and prolong the healing process.
- Don’t engage in high-impact activities such as running or jumping that can further irritate the plantar fascia.
- Don’t wear unsupportive shoes such as flip-flops or high heels that can strain the plantar fascia.
- Don’t self-diagnose or self-treat without the guidance of a qualified healthcare professional.
- Don’t resume high-impact activities too soon after treatment, as this can cause a relapse of symptoms.
RECOMMENDED EXERCISE MACHINES AND BOOKS FOR PATIENT TO BUY FOR THEMSELVES FOR QUICK REHABILITATION IN PLANTAR FASCIITIS
Here are some recommended exercise machines and books for patients with plantar fasciitis:
Exercise Machines:
- Foam roller: A foam roller can be used for self-massage to help alleviate tightness and promote circulation in the feet and calves.
- Foot rocker: A foot rocker is a device designed to stretch the plantar fascia and Achilles tendon. It can help improve flexibility and reduce pain.
- Resistance bands: Resistance bands can be used for strengthening exercises to help improve the stability of the feet and ankles.
- Treadmill: A treadmill with shock-absorbing features can be used for low-impact cardiovascular exercise to improve overall fitness without exacerbating plantar fasciitis.
Books:
- “The Trigger Point Therapy Workbook” by Clair Davies: This book provides detailed instructions on how to use trigger point therapy to alleviate pain and tension in the feet and other parts of the body.
- “The Ultimate Runner’s Guide to Injury Prevention” by Dagny Scott Barrios: This book provides information on how to prevent common running injuries, including plantar fasciitis, through proper training and conditioning.
- “The Complete Guide to Foot Reflexology” by Kevin Kunz and Barbara Kunz: This book provides an introduction to foot reflexology and how it can be used to promote healing and relaxation in the feet and other parts of the body.
It’s important to note that these exercise machines and books are not a substitute for professional medical advice and treatment.
OTHER SIMILAR PHYSICAL THERAPY CONDITIONS RELATED TO PLANTAR FASCIITIS
There are several similar physical therapy conditions that are related to plantar fasciitis, including:
- Achilles tendinitis: This is a condition where the Achilles tendon, which connects the calf muscles to the heel bone, becomes inflamed and painful. It can be caused by overuse or repetitive stress, and often occurs in athletes or individuals who engage in activities that require a lot of jumping or running.
- Heel spurs: A heel spur is a bony growth on the heel bone that can develop as a result of chronic inflammation and irritation of the plantar fascia. It can cause pain and discomfort in the heel, especially when walking or standing for long periods of time.
- Tarsal tunnel syndrome: This is a condition where the tibial nerve, which runs through a narrow tunnel in the ankle, becomes compressed or trapped. It can cause pain, numbness, and tingling in the foot and ankle, and may be related to overuse or repetitive stress.
- Metatarsalgia: This is a condition where the ball of the foot becomes painful and inflamed, often as a result of overuse or wearing poorly fitting shoes. It can cause pain and discomfort in the foot, especially when walking or standing for long periods of time.
Treatment for these conditions may involve similar physical therapy interventions, such as stretching and strengthening exercises, massage, and the use of orthotics or other supportive devices, for more details Connect with Licensed therapist ar Hirephysio.com
FAQ ON PLANTAR FASCIITIS
Q: What is plantar fasciitis?
A: Plantar fasciitis is a common foot condition that occurs when the plantar fascia, a thick band of tissue that runs along the bottom of the foot, becomes inflamed and painful.
Q: What causes plantar fasciitis?
A: Plantar fasciitis can be caused by a variety of factors, including overuse, improper footwear, tight calf muscles, obesity, and biomechanical issues such as flat feet or high arches.
Q: What are the symptoms of plantar fasciitis?
A: The most common symptoms of plantar fasciitis include pain and tenderness in the bottom of the foot, especially near the heel. The pain is usually worst in the morning or after periods of rest, and may improve with activity.
Q: How is plantar fasciitis diagnosed?
A: Plantar fasciitis is typically diagnosed based on a physical examination and a review of the patient’s medical history. Imaging tests such as X-rays or MRIs may be used to rule out other potential causes of foot pain.
Q: What are the treatment options for plantar fasciitis?
A: Treatment options for plantar fasciitis may include physical therapy, stretching and strengthening exercises, footwear modifications, orthotics, anti-inflammatory medications, corticosteroid injections, and in rare cases, surgery.
Q: How long does it take to recover from plantar fasciitis?
A: The length of recovery time for plantar fasciitis varies depending on the severity of the condition and the individual patient. With proper treatment and self-care measures, many patients are able to recover within a few months.
Q: Can plantar fasciitis be prevented?
A: Yes, plantar fasciitis can often be prevented by wearing supportive footwear, stretching regularly, maintaining a healthy weight, and avoiding activities that put excessive stress on the feet.
Q: Can physical therapy help with plantar fasciitis?
A: Yes, physical therapy is often an effective treatment option for plantar fasciitis, as it can help improve flexibility, strength, and range of motion in the affected foot.
Q: What are some recommended treatments for plantar fasciitis?
A: Recommended treatments for plantar fasciitis include rest, ice, stretching exercises, physical therapy, and the use of supportive shoes or orthotic devices. In more severe cases, medications, injections, or surgery may be necessary.
Q: Where can I find a good doctor for plantar fasciitis near me?
A: You can search for a doctor specializing in foot and ankle care or sports medicine in your area. You may also consider seeking a referral from your primary care physician.
Q: What are foot supports for plantar fasciitis?
A: Foot supports, such as arch supports or orthotic inserts, can help alleviate the pain and discomfort associated with plantar fasciitis by providing additional support and cushioning to the foot.
Q: Are compression socks recommended for plantar fasciitis?
A: Yes, compression socks can help improve blood flow and reduce inflammation in the foot, which may help alleviate pain and discomfort associated with plantar fasciitis.
Q: How long does it take to recover from plantar fasciitis?
A: Recovery time can vary depending on the severity of the condition and the treatment method used. Mild cases of plantar fasciitis may heal within a few weeks, while more severe cases may take several months or longer to heal.
Q: What is chronic plantar fasciitis and how is it treated?
A: Chronic plantar fasciitis is a condition where the pain and discomfort associated with plantar fasciitis persists for an extended period of time, typically several months or longer. Treatment may involve more aggressive forms of therapy, such as physical therapy, medications, injections, or surgery.
Q: What is therapy for plantar fasciitis?
A: Physical therapy is a common form of therapy for plantar fasciitis, which may involve stretching exercises, massage, or the use of specialized equipment to alleviate pain and discomfort and promote healing.
Q. What can I do to prevent plantar fasciitis?
A:
- Maintain a healthy weight to reduce the pressure on your feet
- Choose supportive shoes with good arch support and cushioning
- Avoid wearing worn-out or ill-fitting shoes
- Stretch your feet and calf muscles regularly
- Gradually increase the intensity and duration of your
Q. Name some best physiotherapist near me in India (Mumbai, chandigarh,Punjab (mohali, Ludhiana, Machhiwara, Samrala, Kohara)) , Canada, America and worldwide?
A. There are various physiotherapists available near you, but the right physiotherapist is the one who can fasten the rehabilitation process and in many cases help you avoid Surgery. So we recommend Hirephysio.com to hire best physiotherapist or Physical Therapist Doctor near you.
More Articles: